John M. White

John M. White
President/CEO, Protection Management, LLCJohn M. White is the President/CEO of Protection Management, LLC, an independent security consulting firm. John is Board Certified in Security Management as a Certified Protection Professional (CPP), and also a Certified Healthcare Protection Administrator (CHPA). He has over 35 years of security management, law enforcement experience, security consulting, and he has contributed to security related books and trade journals. John specializes in security consulting, security risk assessments, and security planning, and has trained police and security officers in classroom settings as well as on the job.
Security Consulting Security Management Security Operations Starting a Security Department Healthcare Security Emergency Room Violence Security Related Litigation Special Event Security Planning Security/Risk Assessments Vulnerability Assessments Security Operations Reorganization Interim Security ManagementSecurity Training Workplace Violence Assessments Active Shooter Response Training Security Policy Development/Review
News mentions
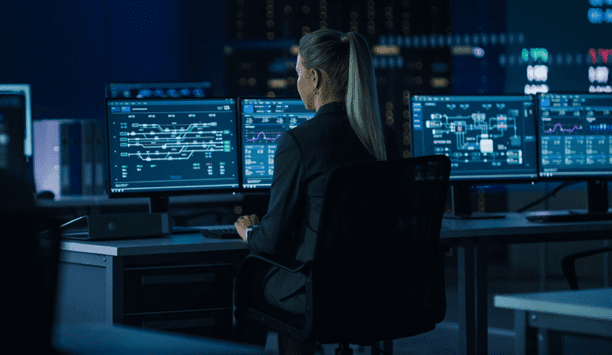
When violence or a life-threatening incident occurs, hospitals and other healthcare institutions are often in the crosshairs. Hospitals increasingly face a reality of workplace violence, attacks on pa...
Spread of the Ebola virus beyond Western Africa has heightened concerns among healthcare professionals and the general public. In practical terms, healthcare facilities – including their securit...